Managing Vision Loss: A Comprehensive Guide to Glaucoma Care
Glaucoma is a group of eye conditions that damage the optic nerve, often due to elevated intraocular pressure. Left untreated, it can lead to irreversible vision loss and blindness. Understanding the available management options, from medications to surgical interventions, is essential for anyone diagnosed with this chronic condition. This guide explores the current approaches to managing glaucoma, the importance of early detection, and what emerging research suggests for the future of care.
Glaucoma affects millions of people worldwide and remains one of the leading causes of preventable blindness. The condition typically progresses slowly, making early detection and consistent management critical to preserving vision. Management strategies vary depending on the type and severity of glaucoma, but the primary goal is always to lower intraocular pressure and prevent further damage to the optic nerve. With advances in medical technology and a better understanding of the disease, patients today have access to a range of effective options.
What Current Research Says About Managing Glaucoma with Medications Laser and Surgery
Current research highlights three main pillars of glaucoma management: medications, laser procedures, and surgical interventions. Medications, primarily in the form of eye drops, remain the first-line approach for most patients. These drops work by either reducing the production of fluid in the eye or improving its drainage. Common classes include prostaglandin analogs, beta-blockers, alpha agonists, and carbonic anhydrase inhibitors. Studies show that consistent use of these medications can effectively control intraocular pressure in many patients.
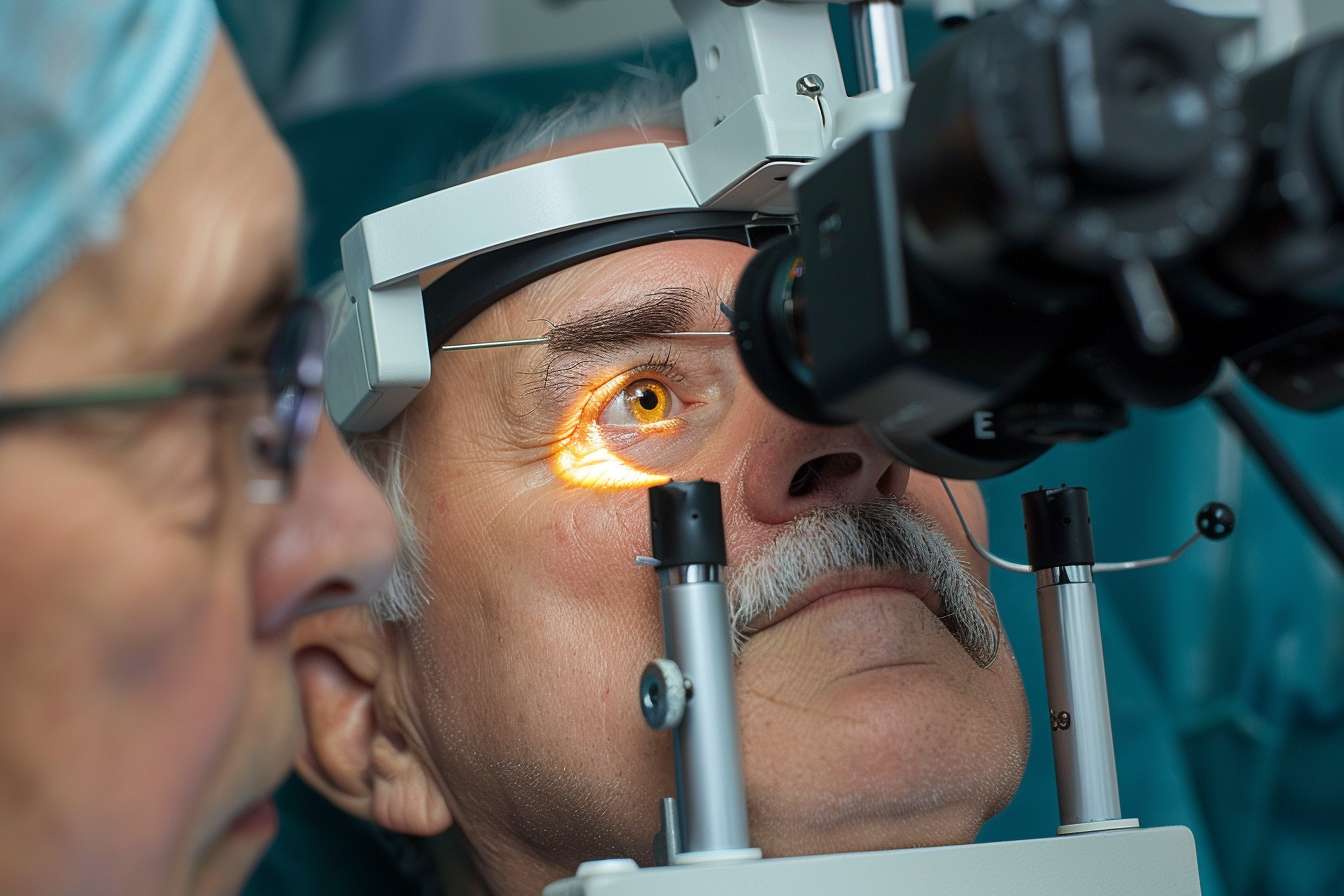
Laser procedures, such as selective laser trabeculoplasty and laser peripheral iridotomy, offer a less invasive alternative when medications alone are insufficient. These procedures improve fluid drainage or create new pathways for fluid to exit the eye. Research indicates that laser therapy can be particularly effective in open-angle glaucoma and may reduce the need for multiple medications.
Surgical options, including trabeculectomy and drainage implants, are typically reserved for more advanced cases or when other approaches fail. Minimally invasive glaucoma surgeries have gained popularity in recent years, offering reduced recovery times and fewer complications compared to traditional procedures. Clinical trials continue to evaluate the long-term efficacy of these newer techniques.
How to Choose the Right Treatment Strategy from Eye Drops to Minimally Invasive Options
Choosing the appropriate strategy depends on several factors, including the type of glaucoma, disease severity, patient lifestyle, and individual response to interventions. For newly diagnosed patients with mild to moderate glaucoma, eye drops are usually the starting point. Your ophthalmologist will consider factors such as potential side effects, dosing frequency, and cost when selecting a medication.
If eye drops prove ineffective or cause intolerable side effects, laser procedures may be recommended. This option is particularly appealing for patients who struggle with medication adherence or prefer a one-time procedure over daily drops. Selective laser trabeculoplasty can be repeated if necessary and does not preclude future surgical options.
For patients with advanced glaucoma or those who do not respond adequately to medications and laser therapy, surgical intervention becomes necessary. Minimally invasive glaucoma surgeries, such as iStent or Xen Gel Stent implantation, offer a middle ground between traditional surgery and less invasive procedures. These can be performed alone or in conjunction with cataract surgery, making them convenient for older patients.
The decision-making process should always involve a thorough discussion with your eye care specialist, who can assess your specific condition and recommend a personalized plan based on the latest clinical evidence.
Why Early Detection and Consistent Follow-Up Are Key to Protecting Your Vision
Early detection of glaucoma is crucial because the condition often develops without noticeable symptoms until significant vision loss has occurred. Regular comprehensive eye exams, especially for individuals over 40 or those with risk factors such as family history, high myopia, or certain medical conditions, can catch glaucoma in its earliest stages.
Once diagnosed, consistent follow-up appointments are essential. Glaucoma is a chronic condition that requires ongoing monitoring to ensure effectiveness and adjust strategies as needed. During follow-up visits, your ophthalmologist will measure intraocular pressure, examine the optic nerve, and assess visual field changes. These evaluations help determine whether the current approach is adequately controlling the disease or if modifications are necessary.
Patients who maintain regular appointments and adhere to prescribed regimens have significantly better outcomes than those who miss appointments or discontinue medications without medical guidance. The progressive nature of glaucoma means that any delay in adjustment can result in irreversible vision loss.
Understanding the Long-Term Commitment to Glaucoma Management
Managing glaucoma is a lifelong commitment that requires patience, diligence, and collaboration with your healthcare team. Unlike acute conditions that resolve with short-term care, glaucoma demands ongoing attention and adaptation. Many patients will need to use eye drops daily for the rest of their lives, while others may require periodic laser procedures or surgical interventions as the disease evolves.
Adherence to prescribed medications is one of the biggest challenges in glaucoma management. Studies show that up to half of patients do not use their eye drops as directed, often due to forgetfulness, difficulty with administration, or side effects. Developing a routine, using reminder systems, and communicating openly with your doctor about any difficulties can improve adherence and outcomes.
The financial aspect of long-term care is also important to consider. Prescription eye drops, regular office visits, and potential procedures represent ongoing expenses. Many patients benefit from discussing cost concerns with their healthcare providers, who may be able to recommend generic alternatives or connect them with assistance programs.
Lifestyle modifications, such as maintaining a healthy diet, exercising regularly, avoiding smoking, and managing systemic conditions like diabetes and hypertension, can complement medical care and potentially slow disease progression.
Emerging Technologies and Future Directions in Glaucoma Care
The field of glaucoma care is rapidly evolving, with exciting developments on the horizon. Researchers are investigating sustained-release drug delivery systems that could eliminate the need for daily eye drops. These implants or injections would provide continuous medication delivery over weeks or months, dramatically improving adherence and convenience.
Advanced imaging technologies, including optical coherence tomography and artificial intelligence-based diagnostic tools, are enhancing early detection and monitoring capabilities. These innovations allow for more precise assessment of optic nerve health and earlier intervention.
Gene therapy and neuroprotection strategies represent promising future directions. Scientists are exploring ways to protect retinal ganglion cells from damage and potentially regenerate damaged optic nerve tissue. While these approaches remain largely experimental, they offer hope for more definitive solutions beyond pressure reduction.
Minimally invasive surgical techniques continue to improve, with newer devices and procedures being developed to provide effective pressure control with minimal risk. Clinical trials are ongoing to establish the long-term safety and efficacy of these innovations.
Telemedicine and remote monitoring technologies are also transforming glaucoma care, making it easier for patients to maintain regular contact with their healthcare providers and potentially catching problems earlier through home-based pressure monitoring devices.
Conclusion
Glaucoma management has come a long way, offering patients multiple effective options for addressing this sight-threatening condition. From traditional eye drops to cutting-edge surgical techniques, the goal remains the same: preserving vision by controlling intraocular pressure and protecting the optic nerve. Success requires a partnership between patient and healthcare provider, with early detection, consistent adherence, and regular monitoring forming the foundation of effective management. As research continues to advance, the future holds promise for even more convenient, effective, and potentially curative approaches. If you have been diagnosed with glaucoma or have risk factors for the condition, working closely with your eye care specialist and committing to long-term management can help protect your vision for years to come.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.




